A lipoedema (lipohyperplasia dolorosa) is a congenital, symmetrical lipodystrophy (maldistribution of fat) that occurs on the limbs and in the hip area. Pain is the main symptom.

Lipoedema is a painful, lipodystrophy that is presumed to be congenital. The condition is generally chronic and tends to affect women and girls on the limbs and in the torso area. Men are only rarely affected.
The condition is accompanied by vague pain, usually during the second half of the day (lipohyperplasia dolorosa). So-called orthostatic oedema are clearly visible on the legs – they are caused by prolonged strain, such as from sitting or standing for long periods. As the torso area is also commonly affected, we refer to this as a systemic disease.
If the aforementioned symptoms are not present, the case is referred to as a lipohypertrophy and is treated in exactly the same way by plastic surgeons. Both conditions are characterised by the swellings and fatty deposits on the legs, which end at the ankle.
The first symptoms of lipoedema usually occur at the end of puberty. But the illness can also take effect at other stages of life.
According to epidemiological studies, around 10% of all women are affected by lipoedema. As little is still known about the causes of this chronic condition – which, incidentally, has nothing to do with the patient’s weight – and it is difficult to make a clear diagnosis as a result, we expect that the actual figure is far higher than this.
If you believe you may be affected, please consult a specialist who has a clear understanding of how to diagnose and treat lipoedema or lipohypertrophy. Alternatively, contact us for a consultation here in Bonn.
For years, patients suffering with disproportionately large trunks and limbs have not been taken seriously by doctors. Despite dietary changes and exercise not leading to any improvements in appearance, the phenomenon has not been recognised as a standalone, even congenital illness.
Besides the “deformed” looking appearance, the permanent heavy feeling and hypersensitivity in the arms and legs has a deep impact on those affected. Their everyday life has to be managed under the most difficult physical and mental conditions with permanent hypersensitivity in the limbs, pain at every touch and a ubiquitous (permanent) tendency to form haematomas. This combination of symptoms means that untreated patients suffer a considerable reduction to their quality of life. Diagnosis is made even more difficult due to the fact that lipoedema acts like a “chameleon”: it appears in different forms, to different degrees and can be both relapsing and progressive. For some patients, the entire leg region is affected, while for others it is just the lower legs. The lipoedema fat can also form in concentrated areas in the hip and thigh regions. There is often a clear correlation between the appearance on the legs, arms and trunk region, which is why it is referred to as a systematic disease within medical circles.
The morphological classification distinguishes between 4 stages:


For years, patients suffering with disproportionately large trunks and limbs have not been taken seriously by doctors. Despite dietary changes and exercise not leading to any improvements in appearance, the phenomenon has not been recognised as a standalone, even congenital illness.
Besides the “deformed” looking appearance, the permanent heavy feeling and hypersensitivity in the arms and legs has a deep impact on those affected. Their everyday life has to be managed under the most difficult physical and mental conditions with permanent hypersensitivity in the limbs, pain at every touch and a ubiquitous (permanent) tendency to form haematomas. This combination of symptoms means that untreated patients suffer a considerable reduction to their quality of life. Diagnosis is made even more difficult due to the fact that lipoedema acts like a “chameleon”: it appears in different forms, to different degrees and can be both relapsing and progressive. For some patients, the entire leg region is affected, while for others it is just the lower legs. The lipoedema fat can also form in concentrated areas in the hip and thigh regions. There is often a clear correlation between the appearance on the legs, arms and trunk region, which is why it is referred to as a systematic disease within medical circles.
The morphological classification distinguishes between 4 stages:
Stage 1: The skin has a smooth and even surface, but subcutaneous fatty tissue is thick and soft with smaller nodules (“polystyrene skin”).
Stage 2: The skin has an uneven surface with indentations. Subcutaneous fatty tissue is thick and increasingly hard with walnut-sized nodules (“mattress skin”).
Stage 3: The skin has an uneven surface. There is a clear increase in circumference with overhanging areas of tissue (“lobules”). Subcutaneous fatty tissue is thick and hard with larger nodules.
Stage 4: Lipoedema combined with a secondary lymphoedema. The disproportionate increase in the size of the limbs often leads to misaligned joints and/or joint degeneration in the later stages.
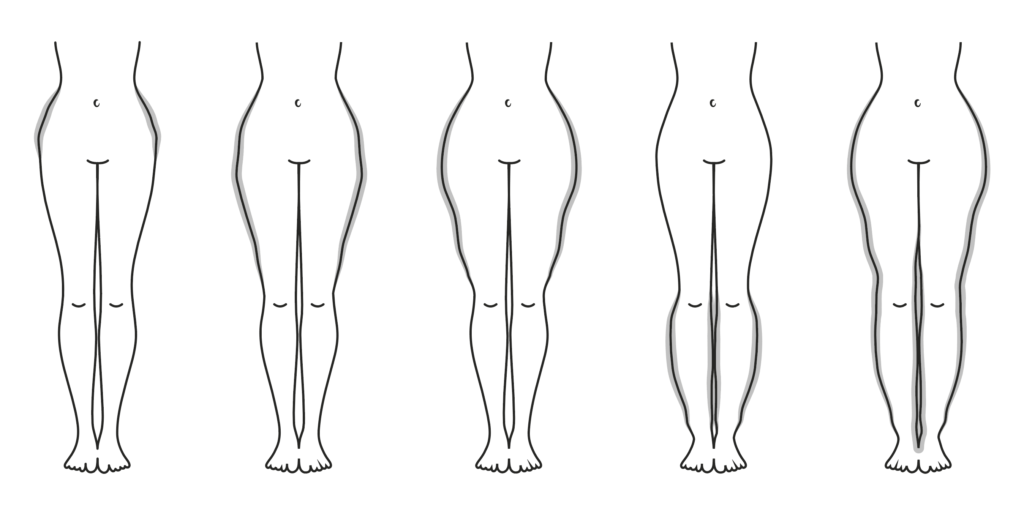
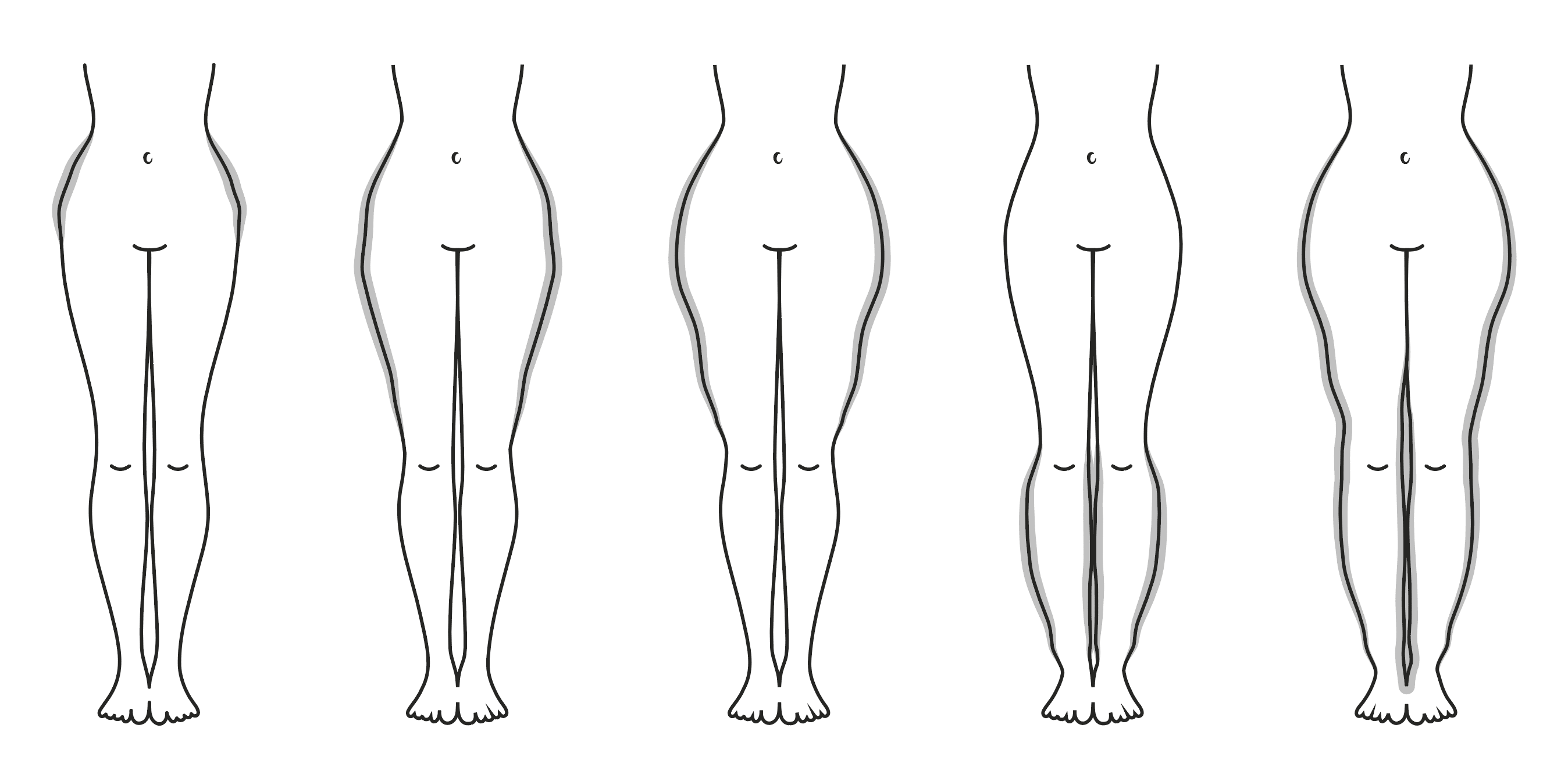
Classification by localisation:
Type 1: Hips
Type 2: Hips and thighs
Type 3: Hips, thighs and lower legs
Type 4: Hips, thighs and lower legs, arms
Classification by region:
Lower extremities: Thigh type, lower-leg type, full-leg type
Upper extremities: Upper-arm type, forearm type, full-arm type
Stage 1: The skin has a smooth and even surface, but subcutaneous fatty tissue is thick and soft with smaller nodules (“polystyrene skin”).
Stage 2: The skin has an uneven surface with indentations. Subcutaneous fatty tissue is thick and increasingly hard with walnut-sized nodules (“mattress skin”).
Stage 3: The skin has an uneven surface. There is a clear increase in circumference with overhanging areas of tissue (“lobules”). Subcutaneous fatty tissue is thick and hard with larger nodules.
Stage 4: Lipoedema combined with a secondary lymphoedema. The disproportionate increase in the size of the limbs often leads to misaligned joints and/or joint degeneration in the later stages.
Classification by localisation:
Type 1: Hips
Type 2: Hips and thighs
Type 3: Hips, thighs and lower legs
Type 4: Hips, thighs and lower legs, arms
Classification by region:
Lower extremities: Thigh type, lower-leg type, full-leg type
Upper extremities: Upper-arm type, forearm type, full-arm type
Unfortunately, we still do not know why patients suffer from lipoedema. We do know that there appears to be a genetic component to the symptoms and that it is almost solely women who are affected by lipoedema. Everything else is currently the subject of research. We hope to know more in the near future.
The lack of a complex picture of the condition means that there is also no causal therapy for lipoedema and, as a result, no promise of a cure. Compression, following a healthy and active lifestyle and – as a last resort – liposuction can help to control the condition. Unfortunate but true: we cannot provide an effective, long-term cure for a condition when we don’t know its cause. But what we do know and what we constantly hear from our patients is this: after long, frustrating periods of conservative therapy, many of them find considerable relief from their symptoms following an operation. As is recommended in the medical guidelines to lipoedema treatment, an operation should be conducted as soon as possible (ideally in stages I-II) so that a sufficient skin retraction can be achieved. It must be ensured that the surgery is performed by an experienced plastic surgeon. Only suitably qualified specialist surgeons have the required level of manual and technical skills thanks to their long and highly specialised training. Specialist surgeons also have a well-trained eye, so they can achieve the best possible results from lipoedema surgery.


Unfortunately, we still do not know why patients suffer from lipoedema. We do know that there appears to be a genetic component to the symptoms and that it is almost solely women who are affected by lipoedema. Everything else is currently the subject of research. We hope to know more in the near future.
The lack of a complex picture of the condition means that there is also no causal therapy for lipoedema and, as a result, no promise of a cure. Compression, following a healthy and active lifestyle and – as a last resort – liposuction can help to control the condition. Unfortunate but true: we cannot provide an effective, long-term cure for a condition when we don’t know its cause. But what we do know and what we constantly hear from our patients is this: after long, frustrating periods of conservative therapy, many of them find considerable relief from their symptoms following an operation. As is recommended in the medical guidelines to lipoedema treatment, an operation should be conducted as soon as possible (ideally in stages I-II) so that a sufficient skin retraction can be achieved. It must be ensured that the surgery is performed by an experienced plastic surgeon. Only suitably qualified specialist surgeons have the required level of manual and technical skills thanks to their long and highly specialised training. Specialist surgeons also have a well-trained eye, so they can achieve the best possible results from lipoedema surgery.
Several different medical conditions have very similar symptoms to lipoedema. These include Decrum’s disease, phlebolymphoedema, benign symmetric Launois-Bensaude type III lipomatosis, primary lymphoedema and lipohypertrophy. As such, it is extremely difficult to clearly diagnose lipoedema. A detailed medical history and physical examination are essential. Typical indications include: the time the first symptoms appeared; a possible familial (genetic) predisposition; the symmetrical distribution of the subcutaneous fat cells with a considerable disproportion between the trunk of the body and the limbs; oedema that progresses (worsens) throughout the day, starting from the ankle upwards; a feeling of heaviness in the legs; a tendency to bruise and the almost unbearable sensitivity to pain when touched, which can be highly problematic, especially in relationships. The initial diagnosis of lipoedema often falls to a doctor specialising in phlebology or a vascular surgeon, who is able to use imaging technology to rule out other possible illnesses and conditions in the venous system. If the oedema go beyond the ankles into the feet, and the skin over the second toe cannot be easily lifted using a “pinching motion” between the thumb and index finger, the so-called “Stemmer sign” is positive and the condition is classed as lipolymphoedema.


Several different medical conditions have very similar symptoms to lipoedema. These include Decrum’s disease, phlebolymphoedema, benign symmetric Launois-Bensaude type III lipomatosis, primary lymphoedema and lipohypertrophy. As such, it is extremely difficult to clearly diagnose lipoedema. A detailed medical history and physical examination are essential. Typical indications include: the time the first symptoms appeared; a possible familial (genetic) predisposition; the symmetrical distribution of the subcutaneous fat cells with a considerable disproportion between the trunk of the body and the limbs; oedema that progresses (worsens) throughout the day, starting from the ankle upwards; a feeling of heaviness in the legs; a tendency to bruise and the almost unbearable sensitivity to pain when touched, which can be highly problematic, especially in relationships. The initial diagnosis of lipoedema often falls to a doctor specialising in phlebology or a vascular surgeon, who is able to use imaging technology to rule out other possible illnesses and conditions in the venous system. If the oedema go beyond the ankles into the feet, and the skin over the second toe cannot be easily lifted using a “pinching motion” between the thumb and index finger, the so-called “Stemmer sign” is positive and the condition is classed as lipolymphoedema.
Lipoedema is generally treated using a combination of different treatments. It is important to note, however, that lipoedema is a chronic, systematic disease that patients unfortunately have to suffer from their entire lives.
Contrary to popular opinion, there is no cure. At present, the following treatments are available:
For diagnoses in the early stages, the so-called complex decongestive therapy has become established among various treatment panels. The aim is to improve the lymph drainage through compression, lymph drainage and movement therapy. In addition, a ketogenic diet has proven effective, as it encourages the metabolism to burn more fat. These measures can be used to slow the progress of the condition, but they can do little to stop the fat cells from multiplying. An operation is the only way to effectively control the lipoedema. In recent years, liposuction has established itself as the only guideline-compliant procedure in this treatment area of plastic surgery.


Lipoedema is generally treated using a combination of different treatments. It is important to note, however, that lipoedema is a chronic, systematic disease that patients unfortunately have to suffer from their entire lives.
Contrary to popular opinion, there is no cure. At present, the following treatments are available:
For diagnoses in the early stages, the so-called complex decongestive therapy has become established among various treatment panels. The aim is to improve the lymph drainage through compression, lymph drainage and movement therapy. In addition, a ketogenic diet has proven effective, as it encourages the metabolism to burn more fat. These measures can be used to slow the progress of the condition, but they can do little to stop the fat cells from multiplying. An operation is the only way to effectively control the lipoedema. In recent years, liposuction has established itself as the only guideline-compliant procedure in this treatment area of plastic surgery.
There are many ways to carry out liposuction. Generally, it comes down to two different procedures: water-assisted liposuction (WAL) and power-assisted liposuction (PAL), which is a very gentle but effective, vibration-enhanced procedure. There are pros and cons to both procedures.
Dr Jorjani is one of the few surgeons in Germany who is highly experienced in both types of operation and is happy to discuss the differences between the two procedures with you in person.
Dr Jorjani is highly specialised in plastic surgery for the treatment of lipoedema. He has operated on thousands of patients (conducting around 500 operations per year) and, as such, has accumulated an enormous bank of experience for all regions of the body.
“Besides the medical requirement to remove as much diseased fatty tissue as possible, I set great store by the final aesthetic appearance. I know that every woman who comes to me for treatment is not just looking to be able to live without pain after their treatment, but is also hoping for a clear improvement in their body shape. We want to use all of our skill to meet this desire – and demand – which is totally justified, in all of the cases that we treat.”


There are many ways to carry out liposuction. Generally, it comes down to two different procedures: water-assisted liposuction (WAL) and power-assisted liposuction (PAL), which is a very gentle but effective, vibration-enhanced procedure. There are pros and cons to both procedures.
Dr Jorjani is one of the few surgeons in Germany who is highly experienced in both types of operation and is happy to discuss the differences between the two procedures with you in person.
Dr Jorjani is highly specialised in plastic surgery for the treatment of lipoedema. He has operated on thousands of patients (conducting around 500 operations per year) and, as such, has accumulated an enormous bank of experience for all regions of the body.
“Besides the medical requirement to remove as much diseased fatty tissue as possible, I set great store by the final aesthetic appearance. I know that every woman who comes to me for treatment is not just looking to be able to live without pain after their treatment, but is also hoping for a clear improvement in their body shape. We want to use all of our skill to meet this desire – and demand – which is totally justified, in all of the cases that we treat.”
The BODYTITE™ process is one of the most effective and modern liposuction methods available for intraoperative skin tightening. Bipolar radiofrequency therapy is used to send energy directly where it is needed – the skin. The skin becomes thicker, more supple and tauter. BodyTiteTM is especially gentle on the lymphatic pathways, nerves and blood vessels.
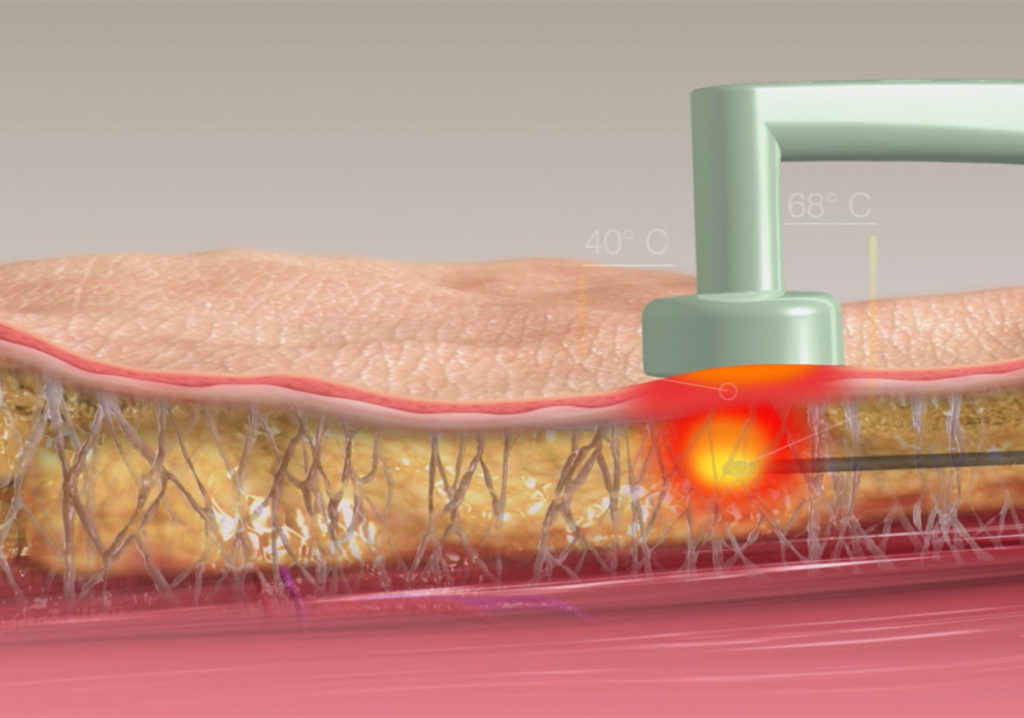

The BODYTITE™ process is one of the most effective and modern liposuction methods available for intraoperative skin tightening. Bipolar radiofrequency therapy is used to send energy directly where it is needed – the skin. The skin becomes thicker, more supple and tauter. BodyTite™ is especially gentle on the lymphatic pathways, nerves and blood vessels.
DAUER
1-3 hours
ANAESTHETIC
Local (tumescent) anaesthetic or general anaesthetic

POST-OP CARE
6-8 weeks
of compression clothing
RECOMMENCE SOCIAL ACTIVITIES
After 2-3 days
EXERCISE
After 6-8 weeks
Most women notice the first symptoms during puberty. Despite no differences to their daily routine, patients suffer from painful swellings, which develop uncontrollably on the arms and legs. The extremities become sensitive to pain and contact. They lose their shape. The upper legs and upper arms begin to sag due to the increasing weight, and gradually start to conceal the elbow and knee joints. The increased mass around the lower legs means that it is suddenly no longer possible to wear boots. In addition, patients have an excess of bruises, as even the slightest touch causes haematoma to form. A permanent sense of heaviness develops. The legs start to feel like permanent weights that you can barely lift. Pronounced relapses of the condition can occur, particular during pregnancy. It is presumed that oestrogen and the female hormonal balance are key factors causing the disease. However, there is no evidence to prove this yet.
Yes. We refer to lipoedema as a “systemic” condition. This means that it can affect the entire body, including the abdomen, back and chin area.
The first step is to talk to a vascular surgeon. We believe that a vascular surgeon is the best person to consult for an initial diagnosis, as they are able to rule out symptoms and can differentiate between lipoedema and lymphoedema. The vascular surgeon will also be able to investigate your circulation and the quality of the flow of blood in your veins. These points are vital when it comes to developing a comprehensive treatment plan for lipoedema. The first stage of therapy also usually begins with the vascular surgeon: compression clothing and manual lymphatic drainage can slow the progress of the condition and are the best way to prepare for any operations that may be required down the line. Important: Please ensure that the vascular surgeon notes down all of their findings and diagnoses in writing. Please bring these documents with you when you visit us for your initial consultation.
Please bear in mind that if you do not have an official diagnosis from a vascular surgeon, consultations and possible operations are viewed as cosmetic surgery by law and are, therefore, subject to VAT.
Of course! The more weight that you can lose prior to the surgery, the better the results will be.
A difficult question. Our experience suggests that the earlier you have the operation, the better. Your skin will thank you for it.
Of course. But you should be aware that lymphoedema can be a chronic condition and that you may need to wear compression clothing for the rest of your life. An operation will generally not make the condition any worse.
In our experience, it is the mental trauma caused by the condition that dictates when an operation is necessary. There are some mild and very slowly progressive forms of the illness and these patients can prevent the condition from developing for many years using conservative therapies and, as such, can still enjoy a good quality of life. Despite this, we do recommend that the operation takes place in the very early stages of the condition, as experience shows that it can considerably slow the progression of the disease.
In recent years, we have enjoyed the extraordinary privilege of being able to perform TAL, PAL and WAL treatments. And there is one thing we can say: there is no perfect therapy. Your surgeon’s level of expertise is what counts when it comes to the results. If performed by an experienced specialist, it doesn’t matter too much which technology you use. The results are usually good and more or less equal. Colleagues who declare that their system is “the best” have not always tested other techniques in sufficient detail. Alternatively, their preferred system may simply be the safest for them to use, so they state their preference based on their results. Water-assisted liposuction (WAL) is, in our opinion, a good and very gentle procedure, which allows for very short operation times, as the local anaesthetic barely needs to take effect. Due to the mostly very pronounced symptoms with lipoedema, the water jet must be used frequently but at a significantly lower pressure during the operation, and sometimes it even needs to be paused – otherwise too much water can be applied to the patient, which can lead to post-operative onset anaemia and circulation issues. In addition, many patients often have severe cramp-like pain after the operation, as the powerful water jet irritates the muscle fascia. In our experience, WAL is a modified and better version of TAL. However, both procedures are undoubtedly very good.
In terms of PAL (power-assisted liposuction), which is the procedure we tend to use, we inject the maximum possible amount of tumescent solution to correspond with the expected fat aspirate at the end of the surgery. In the case of vibration-assisted liposuction, the fat cells dissolve from the cell structures without the use of force. The mechanical irritation of the skin also tends to improve the condition of the skin following the procedure. Here too it is crucial that the surgery is carried out by an experienced surgeon, since unlike other procedures, the constant vibration makes it harder to find the tissue. In our view, the best thing about PAL is that it is possible to use several different cannulas – each suiting different specific regions of the body – so that we can utilise the best tool for each treatment area. Furthermore, we believe that this method is far superior to the other methods when it comes to subsequent liposuction and corrections, as the vibration-based technique allows you to easily move through the scar tissue and patients suffer significantly less pain after the surgery. It should be expressly noted that all findings described here are based on personal experience; they make no claim to being perfect or complete. We can only share what we discovered through our own experience and work – after conducting hundreds of treatments with all 3 techniques.
We are not big fans of absolute numbers. When all things are equal, we can remove up to 10% of the body weight. We usually keep operating until we believe that we have achieved the best result possible. This may be after removing three litres, or it may be after removing eight litres. You need to trust us here. We are a very experienced team and have always demonstrated a good eye for knowing how to achieve the best possible results in the past.
BODYTITE is one of the most effective and modern liposuction methods for intraoperative skin tightening. Bipolar radio frequency therapy is used to send energy directly where it is needed – the skin.
The skin becomes thicker, more supple and tauter. The procedure is especially gentle on the lymphatic pathways, nerves and blood vessels.
You can find out more information about Bodytite here:
https://jorjani.de/en/bodytite/
We currently operate at two locations:
At the Linz-Remagen Hospital (https://www.krankenhaus-linz-remagen.de/informationen-fuer-patienten-besucher/ihre-anreise) and at the
Beethoven Clinic in Cologne (https://www.beethoven-klinik-koeln.de/).
The Linz-Remagen Hospital is a public hospital with its own intensive care unit. The Beethoven Clinic is a private clinic without an intensive care unit.
Both hospitals can provide you with the finest medical care. Treatment at the Linz-Remagen Hospital is only available to patients weighing less than 130 kg, as this is the maximum load capacity of the operating tables on site.
We can only perform leg surgery on patients with a BMI of less than 32 at the Beethoven Clinic in Cologne.
As there is no intensive care unit on site, patients must not be suffering from any relevant secondary illnesses.
It is not possible to state the number of operations required at the start of the treatment. Our rule of thumb is as follows: we will perform as many surgeries as our patients require in order to lead a pain-free and happy life. Sometimes, this can be achieved after just one operation, sometimes it takes four or five. Experience shows that the lower extremities (legs) are best operated on in two sessions (front/rear). The arms and trunk are treated in separate procedures.
Please note that we only combine these surgical areas in the rarest of cases. The flanks, for example, may be combined with the dorsal side of the legs.
By contrast, an operation on the arms cannot be combined with an operation on the legs or abdomen. This is in part due to the size of the resulting wound, but also due to the length of operation that would be required. We treat each area as best we can and that takes time.
We will send you an email around 8 weeks prior to your operation. This email will contain everything that you need to know about the operation itself, how to prepare and your post-op care. The email also includes all the documents that we need from you before we can operate, plus information about insurance to cover any subsequent costs of treatment, and the compression clothing you will require.
We will also send your invoice with this email. Your invoice needs to be paid in full before your surgery.
Prior to the procedure, you will also be contacted to arrange your pre-op consultation. This appointment is used to discuss anaesthesia as well as the procedure for your hospital admission.
Of course not. 99% of our lipoedema patients are women. Please make the necessary preparations, e.g. by bringing hygiene products with you to the hospital.
For reasons of hygiene, we must ask you to please use a tampon or menstrual cup during the operation. You are welcome to switch to a sanitary towel after the surgery.
Please do. You should shave both your legs and your pubic area before surgery. Please ensure that you shave at least 48 hours before your operation.
Towels are provided.
Please inform us / the hospital / the clinic about any food intolerances or allergies at least 14 days before the planned operation.
Only the following are offered:
If we are informed in good time, we can also accommodate intolerances, e.g. to lactose or gluten.
Please bring any special food that you require yourself. Refrigerators are located either on the ward or in the rooms – depending on the ward and where your operation is being performed.
Unfortunately, we cannot take any special requests into account.
As a rule, the procedures take 2 to 3 hours. We only perform liposuction procedures on inpatients. We require patients to be monitored in hospital for at least one night. You will sleep more soundly, and so will we. Smaller operations can be carried out on an outpatient basis in some cases.
As a rule, all incision sites are sewn – our operations are very dry due to the surgical techniques we use, so there is little risk of our patients “leaking” after surgery.
Dr Jorjani generally visits you on the day of surgery and one day after surgery. On subsequent days you will e seen y the on duty medical staff. Dr Jorjani is in constant contact with the ward and is kept up to date. Needless to say, if strictly necessary, Dr Jorjani will pay daily visits.
This varies from patient to patient. Some patients only need to wear compression clothing for 6 to 8 weeks following their operation and can then discard them. Other patients have to wear compression clothing for a lifetime.
Yes. At least twice a week, for 6 to 8 weeks.
Yes. As a rule, they will swell up to their maximum size 14 days after the operation. After that, the treated areas will gradually reduce in size. This can be a quick process, but sometimes it takes longer. Please be patient.
The stitches are removed by us or your GP 10-14 days after your operation
Honestly? We don’t know. This is because the precise cause of the disease is still unknown. What we can tell you, however, is that after the operation many patients enjoy stable long-term results, provided they maintain a healthy lifestyle. After surgery, the metabolism of many patients changes for the better, causing them to lose a lot of weight quite suddenly. The reason for this is also unclear.
This varies from patient to patient and depends on the quality of your skin, your age, level of physical activity and, of course, the amount of fat that we remove. As a rule of thumb, the earlier we can treat your condition, the lower the risk that you will need an additional tightening operation, as younger skin is usually exceptionally good at healing itself. In our clinic, we offer a high level of expertise in liposuction and body tightening, so that we can provide holistic advice and treatment for our patients, including in the event of a worst-case scenario. We use the Bodytite™ system to achieve very good results with minimum excess skin.
Seromas are cavities in the body in which fluid accumulates. They are harmless. They are generally eventually absorbed by the body. However, in some cases they need to be popped. This procedure is usually pain-free, as the skin remains less sensitive due to the liposuction for a relatively long time after the operation, so patients barely feel a thing. Please inform us immediately if you notice any seromas. We can then discuss the next steps together.
Rest assured. This is perfectly normal after such a large-scale liposuction. The normal feeling will return in most cases. It just takes time. In some cases, it can even take a few months.
Aqua jogging, aquafit and gentle swimming are possible 2 to 3 weeks after surgery.
Please wait 4 to 6 weeks post-op before doing any strenuous exercise.
Liposuction for patients with lipoedema is quite unique.
It is important to address the fact that it represents a major intervention which involves risks. The better you are mentally prepared for everything, the easier it will be to deal with the very typical after-effects of the surgery.
Mega liposuction can lead to haematomas, swellings and oedema. Dysaesthesia may occur, especially in the upper and lower legs. Sensations generally return to normal after several months. These sensations may include numbness and tingling.
The risk of hypothermia (where the body temperature falls below 35°C) is increased in comparison with other interventions as larger areas of the body surface are exposed. This can lead to cardiac arrhythmia, coagulopathy, electrolyte imbalances and an increased risk of infection. Thermal regulation in our clinic involves patient warming systems on exposed parts of the body, as well as the prewarming of intravenously administered substances. Furthermore, we provide all patients with antibiotics before and after the operation, without exception, in order to reduce the risk of infection.
For reasons of safety, all of our lipoedema patients are admitted to hospital for liposuction procedures. This means that the vital signs can be monitored on a regular basis during the early stages post-op, and that patients can be mobilised under supervision.
In some cases, haemodilution and post-operative bleeding may cause a symptomatic decrease in the level of haemoglobin. In this case, a transfusion with concentrated red blood cells may be necessary.
We would like to point out that in addition to Dr Jorjani’s proven expertise and level of specialisation in this field, our practice differs from other practices in that we generally perform our operations in a hospital or in a licensed private clinic. We have the option of performing concentrated red blood cell transfusions for the worst-case scenario at both establishments in which we operate.
What does this mean for you?
You will be constantly monitored following the operation. Medical staff will always be on site or nearby and can respond within seconds if required. In the hospital in Linz, we have a large, fully equipped intensive care unit at our disposal, so we can offer treatment to even high-risk patients with a clear conscience.
Rochusstraße 289 | 53123 Bonn
Tel: 0228 – 24 25 54 04
E-Mail: info@jorjani.de
International inquiries:
international@jorjani.de
Mo. | Tu. | Wed. | Thu.
9:00 – 13:00 h
14:00 – 17:00 h
Fr: 9:00 – 14:00 h
Sa: By appointment only